
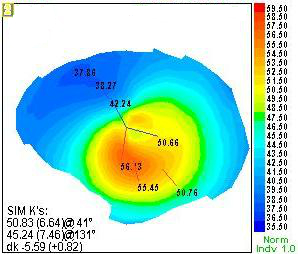
Different surgical techniques are available for PMD management however, none of them were found to be effective, so further studies will be needed in the future. Spectacles, soft and rigid gas permeable contact lens are the main visual correcting method in early stage of the disease. Corneal topography is the main diagnostic tool of PMD with characteristic diagnostic patterns "crab-claw" or "butterfly." PMD could be mistaken as KCN, keratoglobus, and other peripheral thinning conditions such as Terrien marginal degeneration and Mooren's ulcer. It is difficult to differentiate between keratoconus (KCN) and PMD by slit lamp, especially in the detection of early and subclinical stages of the diseases. Pellucid marginal degeneration (PMD) is a rare ectatic corneal disease involving the inferior part of the cornea. At the moment, there is no unanimity with regards to the optimum surgical treatment of PMD and larger prospective studies will be required to form a more robust algorithm for the surgical approach of PMD individuals whose vision cannot be corrected with spectacles or contact lenses. To date, there are no large prospective interventional studies to elucidate the optimum surgical approach for advanced PMD, only case reports or case series.Ĭonclusion: Eye care practitioners need to be aware of the clinical and topographic findings of this disease, since laser refractive surgery is a contraindication. Management of PMD includes the use of contact lenses, spectacles and a wide range of surgical techniques with variable results. PMD patients are at risk of corneal perforation after minimal ocular trauma or even spontaneously. It mainly affects the inferior cornea and induces against the rule irregular corneal astigmatism. Results: PMD is a rare ectatic disorder of the cornea that may resemble keratoconus especially at the early stages. Materials and Methods: Literature review via PubMed, Mendeley, Scopus and Google Scholar. Purpose: To describe the clinical features of Pellucid Marginal Degeneration (PMD) and to give an overview of current treatment options. Poor best-corrected visual acuity at presentation of 0.2 (20/100) or worse and long follow-up (8 years or more) were significantly associated with surgery. Nonsurgical management of PMCD continues to play a predominant role in the management of this disorder. Clear grafts were present in all 10 eyes at the end of the study (average, 9 years SD, +/-82).

Ten eyes (11.8%) underwent penetrating keratoplasty with an average postoperative follow-up of 9 years (SD, +/-8.2 1.5-20.5). Visual acuity of 0.5 (20/40) or better was noted in 34 eyes (75.5%) after contact lens fit. Contact lens management was initially attempted in 51 eyes (60%) however, 7 eyes failed contact lenses. Seventy-five eyes (88.2%) were managed nonsurgically with spectacles in 31 eyes (36.4%) or contact lenses in 44 eyes (51.8%). They were followed-up for an average of 4.7 years (standard deviation (SD), +/-8.7). Information collected from the medical records included demographic data, best-corrected visual acuity, videokeratography, contact lens use, and surgical procedures.įorty-five patients (85 eyes 30 males, 15 females) with PMCD were included in this study. This study was designed to determine how patients with pellucid marginal corneal degeneration (PMCD) are managed in a tertiary corneal practice.Ī retrospective chart review of 45 patients with PMCD from a corneal referral practice was performed.


 0 kommentar(er)
0 kommentar(er)
